IRDAI's tough decision regarding health insurance, claim will have to be settled immediately on death of patient
IRDAI: The Insurance Regulatory and Development Authority of India (IRDAI) said in a circular on Wednesday, that in emergency cases, the insurance company should decide on the request for cashless authorization within one hour of receiving the application. Companies should prepare for this by July 31.

Insurance regulator IRDAI has taken a tough decision regarding health insurance. If the policyholder dies during treatment, the claim will have to be settled immediately. The body will have to be released from the hospital immediately. The regulator has asked insurance companies to achieve 100 percent cashless claim settlement on time.
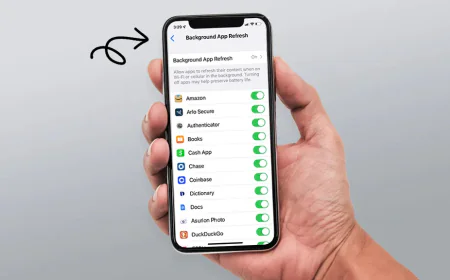
Insurance Regulatory and Development Authority of India (IRDAI) said in a circular on Wednesday, that in emergency cases, the insurance company should decide on the request for cashless authorization within one hour of receiving the application. Companies should prepare for this by July 31. Insurers can set up desks in the hospital to deal with and assist in cashless authorization. The regulator told insurance companies to start the pre-authorization process through digital means. This means that an initial amount has been approved by the insurance company.
If a health claim is made, it cannot be denied without the approval of the PMC, or the PMC's subgroup of three members. The claimant will be fully informed, along with the terms and conditions of the policy document, if the claim is denied or only partially denied.
Want to get your story featured as above? click here!
Want to get your story featured as above? click here!
The company may provide customers with a no claim bonus if there are no claims made during the policy period by raising the insurance amount or lowering the premium amount. Additionally, it has been suggested that customers be given digital tools for quick and easy policy renewal, servicing, and complaint handling.
The policyholder will not need to submit any documents. Insurance companies and third-party administrators i.e. TPA will have to take documents from the hospitals.